Common Misconceptions About Depression

May marks Mental Health Awareness Month. While mental health is important every month, we would like to honour this month by sharing some common misconceptions around mental illness.
Depression in particular is experienced by many individuals – according to Statistics Canada, nearly one in eight adults will meet the criteria for depression at some point in their lifetime.
Recognizing common misconceptions, and knowing the facts, can help us to be gentle with ourselves if we experience symptoms, and to better understand the people in our lives.
People who are depressed cry often
A common misconception is that people who are depressed spend a lot of time crying. Depression presents itself uniquely with each individual – while some people don’t cry at all, some may cry more than others. It truly depends on the person.
In fact, major depressive disorder, or conditions such as post-traumatic stress disorder (which often goes hand in hand with depression), are associated with an inability to cry or feeling numb to emotions.
Regardless of whether people are crying or not, they are still experiencing serious and common symptoms such as:
- Depressed mood,
- Feelings of guilt, worthlessness, helplessness or hopelessness,
- Loss of interest in previously enjoyed activities aka anhedonia,
- Change in weight or appetite,
- Sleep disturbances including excessive sleep, difficulty falling or staying asleep, and nightmares,
- Decreased energy or fatigue without significant physical exertion,
- Thoughts of death and suicide,
- Poor concentration and decision making.
It is important for friends, family members, colleagues, and professionals to understand that just because someone doesn’t cry, doesn’t mean that their experience is invalid or that their depression is any less real, serious, or concerning. People express difficulty in many different ways.
Depression is caused by a bad situation
This isn’t entirely wrong.
 Situational depression is common. This refers to depression that occurs in response to stress related events such as financial or work-related difficulties, interpersonal conflict, being a caregiver for an ill relative, major life transitions, or the death of a loved one. Many people who experience a traumatic event will meet criteria for depression, this can linger if the trauma is not processed.
Situational depression is common. This refers to depression that occurs in response to stress related events such as financial or work-related difficulties, interpersonal conflict, being a caregiver for an ill relative, major life transitions, or the death of a loved one. Many people who experience a traumatic event will meet criteria for depression, this can linger if the trauma is not processed.
Unique to situational depression is clinical depression, also referred to as major depressive disorder. Clinical depression is long-lasting depression without a clear cause. Research continues investigate causes of clinical depression.
Depression, like other mental or physical health problems, can ebb and flow with better and worse days. Being understanding and patient with yourself and/or your loved one is important – depression can be confusing and frustrating, especially when the cause cannot be determined.
Depression only affects women
Everyone can experience depression. Gender does not make one immune. This misconception is one that leads many individuals who do not identify as women to internalize their symptoms and suffer in silence.
It is important to note that research consistently shows that women and LGBTQ+ individuals are more likely than men to experience depression. Women specifically were almost twice as likely as men to have had depression (Anxiety & Depression Association of America), and LGBTQ+ individuals are 2.5 times more likely than their heterosexual peers to experience depression (American Psychiatry Association, Haas et al. 2011).
 Additionally, there are specific forms of depression that are unique to women including:
Additionally, there are specific forms of depression that are unique to women including:
Premenstrual Dysphoric Disorder (PMDD)
A severe form of premenstrual symptoms which brings with it disabling irritability, anger, depressed mood, sadness, suicide ideation, appetite changes, bloating, and pain in the breasts and muscles (National Institute of Mental Health).
Perinatal Depression
Depression that begins during depression (prenatal depression) and depression that begins after the baby is born (postpartum depression). Symptoms include extreme sadness, anxiety, and fatigue interfering with daily tasks (National Institute of Mental Health).
Perimenopausal Depression
Irritability, anxiety, sadness, and loss of enjoyment in life while transitioning into menopause (National Institute of Mental Health).
LGBTQ+ folks are thought to be at higher risk of depression related to high rates of discrimination, stigma and victimization (Canadian Mental Health Association).
It is easy to tell when someone is depressed
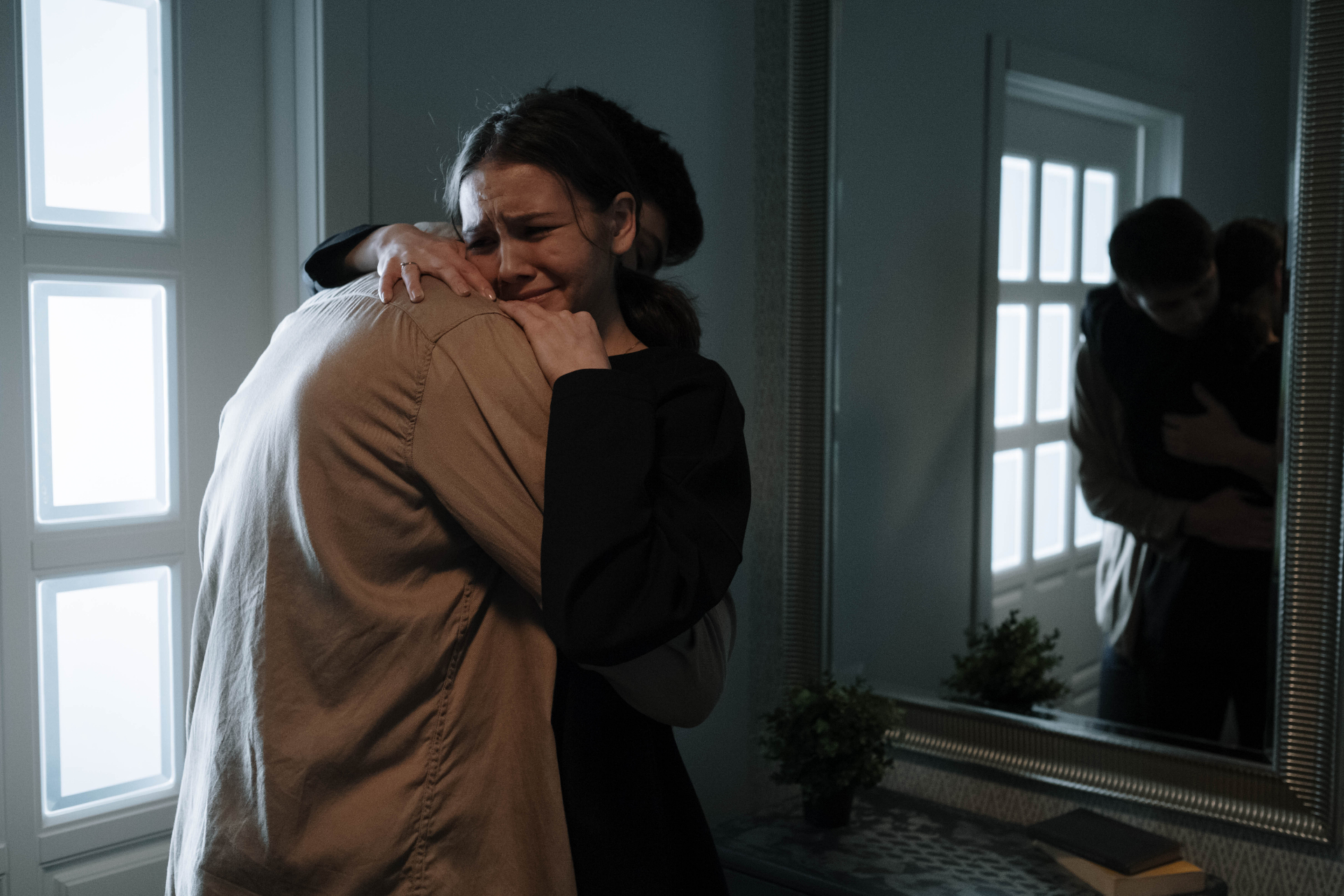
When we hear the word depression it’s common to think of someone who actively shows they are sad. For example, we think of someone with a slouched posture, walking slow, withdrawing, and crying. This description is more typical to sadness than specific to depression.
The truth is that it’s not easy to tell if someone is depressed simply by looking at them. Many individuals with depression continue to work and attend social gatherings while putting on a smile. They may also be checking in on their loved ones while needing support themselves.
Other times depression can manifest itself as anger and substance use.
It is important to remember that it can be hard for someone to open up about depression, because of their own personal beliefs and society’s stigmas. The best way to know if someone is doing okay is to check in with them, and provide support as best you can (this includes checking in on those who might seem just fine).
There’s no treatment for depression
This misconception is dangerous because it can increase feelings of hopelessness and increase suicide ideation. It also prevents people from getting the help they need.
 The reality is that depression is a treatable condition. Extensive research has been done to understand effective treatments which typically includes a medication and/or psychotherapy. Lifestyle changes and improved self-care can improve the outcomes of these interventions.
The reality is that depression is a treatable condition. Extensive research has been done to understand effective treatments which typically includes a medication and/or psychotherapy. Lifestyle changes and improved self-care can improve the outcomes of these interventions.
There is no one size fits all approach – decades of research have shown us that people respond in different ways to different forms of treatment. If you’ve tried one form of therapy with minimal benefit, try another. If one medication didn’t work, there may be another one that does.
Please know that help is available and that you do not have to continue suffering. Make sure to reach out to a regulated health professional for support and to begin your healing.
The points outlined in this blog only begin to scratch the surface of common misconceptions about depression. We encourage you to continue learning about mental health to better understand your own and your loved ones’ experiences.
If you hear anyone spreading these misconceptions, politely share your knowledge with them – they likely don’t know what you now know.


